Human Dependent ECG vs Algorithm Mobile Telemetry?
The prevalence of human factor errors has been determined through either retrospective or prospective research, clinical auditing, and voluntary reporting methods. In a study of 359 preventable adverse occurrences, 359 interviews were conducted. Over 80% were caused by human mistakes. 19% of these occurrences were caused by errors largely involving interface with the anesthetic equipment, while 4.5% were caused by monitoring errors.
Since the ability to detect and correct errors are critical in establishing successful, goal-directed behavior, especially in a cognitively complex environment such as hospitals. The discussion of the accuracy of humans or machines becomes paramount.
The Argument: Which is More Accurate?
Vital signs data are often recorded on paper charts placed at the end of patients' beds or in their rooms. These processes are prone to error and/or failure, such as insufficient monitoring frequency, incomplete data, inaccurate calculations of the early warning score (EWS), and poor chart legibility and interpretability, all of which have been linked to the failure to recognize and respond to patient deterioration.
A recent clinical trial discovered that human-oversight-dependent continuous electrocardiography (ECG) monitors detect severe arrhythmias more accurately than artificial intelligence (AI) algorithm-based mobile cardiac monitoring devices or telemetry (MCT).
So which is it? Let's find out.
The Issue at Hand in Cardiac Monitoring Devices: Human or Equipment?
Over the course of a half-century of ambulatory ECG monitoring, clinicians have rarely had insight into the enormous number of hidden variables that influence the quality of the ECG report on which their medical judgments are based. Algorithm performance is determined by a number of factors, including circuit board design, electrode design and location, signal processing, embedded algorithms, analysis software and heuristics, data transmission techniques, and, most importantly, the presence or absence of human readers of digital data in part or in full. This makes it difficult to compare different brands of ambulatory cardiac monitoring devices side by side without knowing their individual ECG features and algorithms.
The `ideal monitor` for vital signs should be sensitive enough to record significant rhythms while also being specific enough that the end result tracings and relevant context (onset, offset, heart rate trends) presented to the reader allow for correct rhythm diagnosis. Due to their accuracy, portability, and ability to transmit data wirelessly, there has been an explosion of both medical grade (i.e., FDA approved) and commercial grade ambulatory cardiac monitoring technology (e.g., watches, clothes, etc.) in the last ten years. Much of the industry's attention has been focused on ease of use, recording duration, and method of report delivery to the physician, i.e., "real-time" vs. not.
A recent clinical experiment found that when people examined monitoring versus algorithmic monitoring to flag occurrences, detection increased by 209%. This study was conducted in an outpatient arrhythmia clinic and involved 50 consecutive patients who wore both an MCT and a long-term continuous ECG monitor at the same time.
Technology is a human-made, tool-like resource that was initially created to support human activity. To put them against each other would be counterproductive.
But to answer the question for answer's sake. Technology, when combined with critical human monitoring and input, proved to be the most reliable in detecting significant arrhythmias and, ultimately, helping to improve patient outcomes.
According to research, a good cognitively ergonomic design of monitoring equipment for use in these situations could reduce human factors errors linked with the information it provides.
Human Touch in Algorithm Cardiac Monitoring Device
In the end, while the focus of human factor studies has shifted in recent years from instrument design to organizational challenges, patient monitor designers continue to play a vital role in enhancing the safety of the monitored patient. Furthermore, a deeper psychological knowledge of the causes of human factor errors will lead to better human factors engineering in the future.
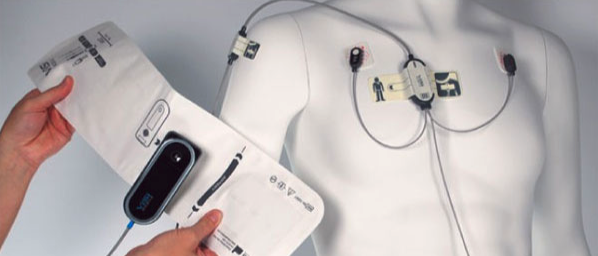
ViSi Mobile, is a continuous vital signs monitoring device that has an algorithm based on millions of hours of patient data to recognize patient deterioration while minimizing alarm burden and maximizing clinical workflow. This algorithm is constantly being updated to provide accurate data and ensure rapid and quality care.

