Detecting and Monitoring Lethal Cardiac Rhythms
Abnormal cardiac rhythms, also known as arrhythmias, can lead to sudden cardiac death if not detected and treated promptly. Wireless monitoring technology offers a solution by providing real-time monitoring and alerts, allowing for timely intervention and potentially saving lives.
In certain instances, emergency medicine and critical care necessitate prompt diagnosis and response. Accurate detection of abnormal cardiac rhythms that are lethal is critical for appropriate therapy in cardiac crises. Many times, patients with underlying arrhythmias are unaware of the issue, and only subtle hints from the physical examination prompt further investigation with a 12-lead surface electrocardiogram.
Symptoms of Lethal Cardiac Rhythms
Lethal cardiac rhythms, also known as lethal arrhythmias, are a serious medical concern that can have varying causes and outcomes. While some individuals may be aware of their irregular heartbeats, known as palpitations, the severity of an arrhythmia is not always directly related to the symptoms it generates.
In fact, some arrhythmias may have no signs, while others with minor consequences may have severe symptoms. The underlying heart disorder and its form and severity are often more critical than the patient understands since they aren’t having significant symptoms. Arrhythmias can lead to weakness, decreased ability to exercise, shortness of breath, lightheadedness, dizziness, fainting, and even death if blood clots form and begin circulating, impeding blood flow to the lungs (pulmonary embolism) or brain (embolic stroke). It is important to seek treatment for arrhythmias that cause symptoms as soon as possible. [1,4]
Detecting Lethal Cardiac Rhythms
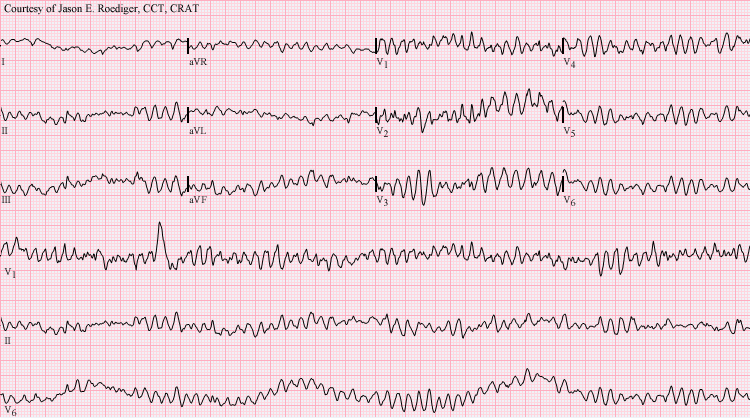
There are a few simple ways to detect lethal cardiac rhythms. The most reliable way is through an electrocardiograph (ECG), which can detect cardiac ischemia up to several hours after they have occurred. [3]
Cardiac arrhythmias, such as atrial fibrillation, are prevalent and can lead to serious complications, such as embolic stroke. Less common but more dangerous rhythm problems, such as ventricular tachycardia, can signal the onset of sudden cardiac death (SCD). Arrhythmia detection and care in patients with palpitations, syncope, a history of arrhythmia, or a high risk for SCD frequently rely on conventional Holter monitoring, event monitoring, or continuous remote telemetry. [1,2]
While helpful, these technologies are burdensome for the patient, costly (up to $750), and frequently miss arrhythmias if the patient does not activate the event monitor at the time of their symptoms. A number of novel and effective wireless arrhythmia monitoring methods have been developed and verified, and are now available for patient care. [1]
Cardiac patients on telemetry wards require close monitoring, including frequent vital sign measurements and ECG monitoring. The most seriously ill patients, on the other hand, have their vital signs measured and reported to their doctors just every 15 minutes in the ICU. Less critical patients are monitored every 4-6 hours on the telemetry units. Recent improvements in non-invasive blood pressure monitoring and wireless delivery systems have enabled all in-patients to get continuous vital sign monitoring in the form of a compact monitor slightly larger than a wrist watch. [1]
Wireless Monitoring of Lethal Cardiac Rhythms
The ViSi mobile system from Sotera consists of a patient-worn monitor that is linked to a series of small biosensors such as a pulse oximeter, skin temperature sensor, telemetry leads, and a non-invasive continuous blood pressure monitor that uses pulse arrival time (PAT) and cuff calibration to continuously monitor the patient.
The PAT is defined as the time it takes for the arterial pulse pressure wave to travel from the aortic valve to the periphery and can be calculated as the difference between the peak of the R wave on the ECG and the arrival of the equivalent pulse wave on pulse oximetry (photoplethysmography). It has been verified in a variety of circumstances as an accurate approach for non-invasive blood pressure measurement.
The technique of calculating blood pressure using Pulse Arrival Time can result in pushback from bedside staff since it is new and different from traditional blood pressure measuring on general care floors. To alleviate their concerns, staff are educated about how the ViSi Mobile System uses accelerometers, time synchronized sensors and notifications as listed below, to ensure accuracy within +/- 5 mmHg of an invasive arterial blood pressure measurement:
- Accelerometers are used to correct for inaccuracies caused by hydrostatic pressure changes and the pre-ejection time.
- The calibration step determines a patient's unique cardiovascular profile.
- Time-synchronized sensors produce a consistent link between pulse arrival time and blood pressure.
- The user is notified if there are significant variations in mean arterial pressure.
ViSi Mobile is more than just a vital sign and cardiac monitoring system. It can wirelessly communicate data to the electronic medical record and remote alarm systems via secure encryption over current Wi-Fi networks, giving the physician 24-hour access to all of the patient's important vital signs.
More information about ViSi Mobile's dependability can be found in the many published clinical studies compiled here.
Sources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4135373/
https://www.mayoclinic.org/diseases-conditions/heart-arrhythmia/symptoms-causes/syc-20350668
https://www.mayoclinic.org/diseases-conditions/heart-arrhythmia/diagnosis-treatment/drc-20350674
https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/arrhythmia/types.html

